The correct measurement, assessment and understanding of body temperature is important for maternal and child health. To that effect, Braun has developed the ThermoScan® 7, an innovative ear thermometer that helps parents to interpret temperature measurements.
According to the NHS as ‘a general rule, a temperature of 38C (100.4F) or above is classified as a fever in children’ (NHS Choices, 2016a).
The NHS recommends seeking medical advice if:

Fever is the body’s natural response to fighting infection. There’s a twofold reason our bodies respond in this way [1]. Firstly, and perhaps the best-known purpose that we develop a fever, is that an increased body temperature helps the immune system work more effectively. Studies have shown that our infection fighting white blood cells are stimulated and there is an increased production of antibodies when our temperature is higher. This is our body’s immediate and highly effective way of fighting infection.
The second purpose for a fever is that elevated heat levels within the body have been found to slow down, and in some cases stop, the growth and reproduction of some kinds of bacteria that can’t function in warmer environments. When combined, the body warming and a fever ensuing can be an effective way to fight infection fast.
The dilemma lies, as to at what point the fever should be treated. It is the body’s natural response and while your little one will feel uncomfortable for a short while, the fever is actually helping their body fight the infection. While it may be upsetting to see your child hot and bothered, it is actually their body doing what it needs to in order for them feel well again.
NICE (2013) does not recommend using antipyretic medicines solely for the purpose of reducing body temperature in children with a fever, or preventing febrile seizures, as there is no evidence to suggest they decrease the risk of seizures (NICE, 2013). However if your child is distressed or in pain you can treat them with the appropriate dose of paracetamol or ibuprofen syrup.
That said, it is important to know the symptoms to watch that can accompany a fever. If the child at any point has a headache, muscular pain or becomes unresponsive it is important to see a doctor immediately.
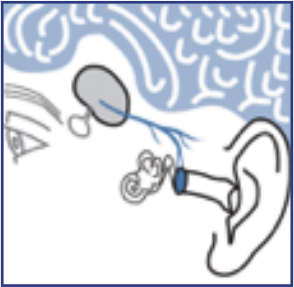
The ear can be a good site for temperature measurement because it reflects the core temperature of the body [2]. Body temperature is regulated by the hypothalamus [3], which shares the same blood supply as the tympanic membrane (which is in the ear). Changes in core body temperature can usually be detected sooner in the tympanic membrane [4] than in other sites, such as the rectum, mouth or under the arm.

The Braun ThermoScan® 7 Ear thermometer includes Age Precision® technology that takes age into account when showing the temperature on its colour-coded display. This helps parents in understanding more easily if the temperature reading is normal (green), fever (yellow) or high fever (red).
With its patented pre-warmed soft tip, you will also value the professional accuracy and precision that the Braun ThermoScan® 7 gives you.
Trust the thermometer brand that 8 out of 10 doctors recommend [6].
Visit www.brauntherms.com for more information about the Braun Thermometers product range and where they are available, as well as more insights about fever.
[1] https://www.britannica.com/science/fever
[2] GUYTON A C, TEXTBOOK OF MEDICAL PHYSIOLOGY, W.B. SAUNDERS, PHILADELPHIA, 2016, P 919.
[3] GUYTON A C, TEXTBOOK OF MEDICAL PHYSIOLOGY, W.B. SAUNDERS, PHILADELPHIA, 2016, P 754-5
[4] NETTER H F, ATLAS OF HUMAN ANATOMY, NOVARTIS MEDICAL EDUCATION, EAST HANOVER, NJ, 1997, PP 63, 95.
[5] Loveys, A A / Dutko-Fioravanti, I / Eberly, S W / Powell, K R.Comparison of ear to rectal temperature measurements in infants and toddlers Clinical Pediatrics, Volume: 38 Issue: 8, page(s): 463-466. 1999.
[6] Of the 27% of respondents who recommend a certain brand. Source: Ipsos, online study among n=802 GPs and Pediatricians in four European markets (n=200 each in GE, UK, FR, NL), fielded in Jan-Feb 2017.